Low adherence to secondary prevention medications (ATM) of patients after acute coronary syndrome (ACS) is associated with poor clinical outcomes. However, literature provides limited data on assessment of ATM and risks associated with poor in Chinese patients with ACS. In the current work, ATM was assessed in consecutively recruited patients with ACS in Tongji Hospital from November 5, 2013 to December 31, 2014. A total of 2126 patients were classified under low adherence (proportion of days covered (PDC)<50%) and high adherence (PDC>50%) groups based on their performance after discharge. All patients were followed up at the 1st, 6th, and 12th month of discharge while recording ATM and major adverse cardiac events (MACE). Bivariate logistic regression was used to identify the factors associated with ATM. Cox regression was used to analyze the association between ATM and MACE within one year after discharge. Results showed that coronary artery bypass grafting (CABG) alone had significantly lower proportion of high adherence to P2Y12 antagonists (83.0% vs. 90.7%, P<0.01) than patients treated with percutaneous coronary intervention (PCI) only. Moreover, in patients undergoing PCI, high adherence to P2Y12 antagonists decreased the risk of MACE (hazard ratio=0.172, 95% confidence interval: 0.039–0.763; P=0.021). In conclusion, PCI-treated patients are more prone to remaining adherent to medications than CABG-treated patients. High adherence to P2Y12 antagonists was associated with lower risk of MACE.
Coronary heart disease (CHD) remains to be a leading cause of global mortality [1]. Acute coronary syndrome (ACS), a severe CHD, consists of non-ST-segment elevation myocardial infarction (NSTEMI), ST-segment elevation myocardial infarction (STEMI), and unstable angina (UA) [2]. The 2015 ESC Guidelines and 2016 ACC/AHA Guideline recommend dual antiplatelet treatment (DAPT), statins, angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin II type 1 receptor blockers (ARBs), and b-blockers for patients with ACS [2,3].
However, underuse of medications is prevalent in patients with ACS and may involve therapy prevention, low adherence, and underdosing. Low adherence remains complex, ill-characterized, and unpredictable. In the study by Gislason et al. [4], only 58%, 74%, and 82% of ACS patients who survived were still adherent to b-blockers, ACEIs/ARBs, and statins after five years of post-discharge, respectively. Similarly, nearly one-third of myocardial infarction (MI) patients discontinued taking at least one of their prescribed medications by the 6th month in TRANSLATE-ACS study [5].
To overcome low adherence to secondary prevention medications (ATM), identifying risk factors is essential. Many factors, such as demographics, comorbidities, and medication class, contribute to ATM [4]. Furthermore, in an observational study, prescription coverage of clopidogrel dropped after percutaneous coronary intervention (PCI), which is associated with increased risk of major adverse cardiovascular events (MACE). Similarly, Jari et al. demonstrated that long-term use of statins was associated with decreased risk of CHD mortality [6]. However, low ATM and MACE still manifest vague association. Ferreira-Gonza’lez et al. observed that during the first year after PCI, discontinuation of antiplatelet medications (aspirin or P2Y12 antagonists) is usually temporary and does not markedly worsen the outcome [7].
Despite numerous studies, literature provides limited information on ATM of Chinese patients with ACS. Thus, we conducted this prospective cohort study to identify the factors associated with ATM and assess risks of low ATM in Chinese patients with ACS.
This work was designed as a prospective follow-up study. All patients diagnosed with ACS upon discharge and at the age of 18 years or older were enrolled at Tongji Hospital, Tongji Medical College in Wuhan from November 5, 2013 to December 31, 2014. ACS involves MI (NSTEMI and STEMI) and UA. MI is defined as cardiomyocyte necrosis in clinical setting and is consistent with acute myocardial ischemia; UA is defined as myocardial ischemia at rest or minimal exertion without cardiomyocyte necrosis [2]. Excluded from the study were patients with metastatic cancers or died prior to 30 days after discharge or who were not followed up.
We developed an initial case report form and subsequently finalized it for field use after pilot testing. Information was collected using baseline characteristics on demographics (age, gender, education level, and types of medical insurance), comorbid conditions, history of atrial fibrillation, heart failure, stroke, implantable cardioverter defibrillator (ICD), radiofrequency ablation, chronic renal dysfunction (CRD), types of ACS (STEMI, non-STEMI, and UA), and ACS treatment, which consisted of PCI, coronary artery bypass grafting (CABG), combined PCI and CABG treatment (hybrid procedure), and conservative treatment from medical records or personal interviews with patients. Case report forms were completed by trained hospital staff using EpiData Software Version 3.1. A unique and permanent civil number was used to identify the patients enrolled.
All patients who enrolled voluntarily signed written informed consents and were interviewed by phone and face-to-face by trained researchers at the 1st, 6th, and 12th month after discharge using a standardized questionnaire to determine vital status, current medications (patients were asked to collect all their current medications and to read out every brand name), date, and reason for hospital readmissions. When a patient died, a close relative was interviewed. In case of readmission, clinical records were reviewed to establish reasons for readmission and medications during hospitalization and at discharge.
We registered each patient’s discharge medications, including aspirin, P2Y12 antagonists, statins, ACEIs/ARBs, and b-blockers from medical records. P2Y12 antagonists in this study were clopidogrel hydrogen sulfate, ticagrelor, and clopidogrel bisulfate. The statins were atorvastatin calcium (produced by Pfizer or Jarlin in Beijing), rosuvastatin calcium, and others. The ACEIs/ARBs were ACERTIL (perindopril), fosinopril sodium, benazepril hydrochloride, perindopril and indapamide (BIPREL forte), valsartan capsules, telmisartan, irbesartan, and others. The b-blockers were metoprolol succinate sustained-release tablets and Concor (bisoprolol fumarate). We assessed the adherence to each medication of each patient by calculating the proportion of days covered (PDC), which was considered to measure patients’ ATM [8]. The PDC for each medication is defined as the days that patients were provided with filled prescriptions divided by the 12-month observational time interval or first day after discharge to the day of the last interview. The days when patients were given filled prescriptions started from the first day after discharge to the last day, unless they stopped taking medications for at least three months. From phone and face-to-face interviews and from reviews of clinical records, we recorded discontinued medications and approximate date of interruption. Thus, the approximate PDC could be determined for each patient and each medication. We also classified the patients under low adherence (PDC<50%) and high adherence (PDC>50%) groups.
We recorded the occurrence of MACE for 12 months after discharge given that one year is the recommended duration for effects of P2Y12 antagonists. MACE was defined as the first occurrence of cardiovascular death, MI, and revascularization.
Cardiovascular death was defined as any death resulting from cardiac-related conditions (e.g., MI, low-output failure, and fatal arrhythmia), unwitnessed death, death of unknown cause, and all procedure-related deaths, including those related to concomitant treatment [9].
Myocardial infarction is defined by pathology as myocardial cell death due to prolonged ischemia. [10].
Revascularization is defined as any percutaneous intervention or surgical bypass. An independent angiographic core laboratory verified whether severity of percent diameter stenosis met the requirements for clinical diagnosis; the laboratory could overrule in cases wherein reports were not in agreement [9].
All outcomes were identified from clinical records and phone interviews by the main investigator team, who were blind to medication adherence status by the end of adjudication.
For continuous variables, results were expressed as mean values±SD. We used frequency statistics to summarize baseline population characteristics (demographics, medical insurance types, comorbid conditions, ACS types, ACS treatment types, cardiovascular history, and concomitant treatment). Chi-square test was used to compare groups and to identify significant differences in their adherence to each medication. Regression analysis was conducted using PDC as bivariate measurement (low adherence vs. high adherence). Multivariate logistic regression was used to evaluate independent associations between concomitant medications and adherence to aspirin, P2Y12 antagonists, ACEIs/ARBs and b-blockers after adjustment for ACS treatments for PCI, CABG, combined PCI and CABG, and conservative treatment, respectively, using forward: LR. For statins, adherence was adjusted for ACS types and radiofrequency ablation.
We used Kaplan–Meier curves to determine one-year cardiac MACE rates and Cox regression modeling to assess whether low ATM was associated with higher risk of MACE. Hazard ratios were adjusted for potential confounders (ACS treatment, radiofrequency ablation, and concomitant treatments) using multivariate Cox regression analysis (forward: LR). For the PCI population, hazard ratios were merely adjusted by concomitant treatments. Finally, data were assessed by power analysis (a = 0.05) using PASS Version 11.
All statistical calculations were performed using the Statistical Package for Social Sciences (SPSS) Version 22.0. All P values<0.05 were regarded as statistically significant.
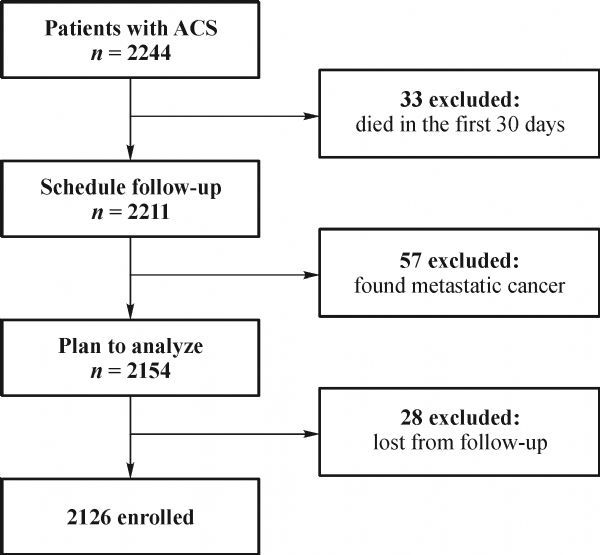
Fig. 1 shows the flowchart for the study population. A total of 2244 patients with ACS in Tongji Hospital from November 5, 2013 to December 31, 2014 were included in the study. Among the 2244 patients, 33 died in the first 30 days after discharge, 28 were missed during follow-up. The 57 patients who were excluded were diagnosed with metastatic cancer during the follow-up. The final study population consisted of 2126 patients. Among the 2032 (95.6%) patients, follow-up was achieved at three time points (1st, 6th, and 12th month), and only two follow-up time points (1st month and the last phone interview) were available for the rest. Among the selected patients, 2058 (96.8%) had prescriptions for aspirin, 1840 (86.5%) for P2Y12 antagonists, 2081 (97.9%) for statins, 1460 (68.7%) for ACEIs/ARBs, and 1578 (74.2%) for b-blockers at discharge (Fig. S1). Among patients with at least one prescription filled, 1937 (94.1%), 1681 (91.4%), 1927 (92.6%), 1201 (82.3%), and 1367 (86.6%) patients remained adherent to aspirin, P2Y12 antagonists, statins, ACEIs/ARBs, and b-blockers, respectively, at the 6th month. By the 12th month, 1846 (89.7%), 1523 (82.8%), 1795 (86.3%), 998 (68.4%), and 1221 (77.4%) patients remained adherent to aspirin, P2Y12 antagonists, statins, ACEIs/ARBs, and b-blockers prescribed after discharge, respectively (Fig. S2). For P2Y12 antagonists, 1704 patients took clopidogrel hydrogen sulfate, 116 had ticagrelor, and 20 patients took clopidogrel bisulfate. For statins, 1715 patients took atorvastatin calcium, 334 patients had rosuvastatin calcium, and 32 patients took other types of statins. For ACEIs/ARBs, 1064 patients took perindopril (ACERTIL), 230 had fosinopril sodium tablets, 92 patients took benazepril hydrochloride, 11 patients took perindopril and indapamide (BIPREL forte), and 40 patients received valsartan capsules. For b-blockers, 1430 patients took metoprolol succinate sustained-release tablets, and 146 patients took bisoprolol (Fig. S3).
Fig.1 Flowchart of study cohort identification and exclusion. ACS, acute coronary syndrome.
Table 1 shows the baseline characteristics of the study population. The cohort included 384 patients with acute STEMI, 273 with acute NSTEMI, and 1469 with UA. Among the patients, 1616 (76.0%) patients were treated with PCI only, 73 (3.4%) received CABG treatment only, three (0.1%) had combined PCI and CABG treatment (hybrid procedure), and 434 (20.4%) patients were treated conservatively. Tables 2 and S1–S4 showed that patients with history of radiofrequency ablation were more prone to remaining highly adherent to statins than patients without radiofrequency ablation. (99.6% patients with radiofrequency ablation vs. 97.4% without radiofrequency ablation, P = 0.021). PCI-treated patients had higher adherence to aspirin (97.4% vs. 88.0%, P<0.01), P2Y12 antagonists (97.5% vs.78.3%, P<0.01), statins (96.2% vs. 87.3%, P<0.01), and b-blockers (90.7% vs. 84.6%, P<0.01). Furthermore, compared with PCI-only-treated patients, CABG-only-treated patients had significantly lower proportion of high adherence to P2Y12 antagonists (83.0% vs. 90.7%, P<0.01), and our power (1-β) has attained 1.00. No relevant differences concerning psychosocial characteristics were observed between the two groups.
Fig.S4 shows that patients taking aspirin had lower probability for discontinuing use of statins and b-blockers (ORstatins = 0.26 [0.12, 0.55] and ORβ-blockers = 0.38 [0.17, 0.84]). The concomitant use of P2Y12 antagonists improved the adherence of patients to aspirin and statins (ORstatins = 0.29 [0.18, 0.46] and ORβ-blockers = 0.38 [0.25, 0.58]). On the contrary, the adjusted logistic regression model revealed that concomitant medication was not significantly associated with adherence.
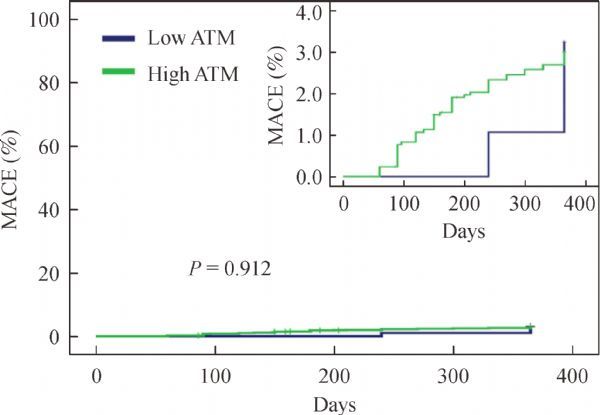
Risk of MACE and low ATM did not show significantly different association; the same result was still observed after adjustment for potential confounders (Table 3, Figs. 2, and S5–S8).
Fig.2 Estimated rates of MACE per adherence to P2Y12 antagonists in ACS population. The panel shows outcomes of the study population. X-axis presents days after discharge and Y-axis indicates cumulative rates of MACE. The inset graph in each panel shows the same curves on a larger scale. MACE: major adverse cardiac events.
Among the 1616 patients undergoing PCI only, 1598 (98.9%), 1570 (97.2%), 1601 (99.1%), 1168 (72.3%), and 1239 (76.7%) patients had filled prescriptions for aspirin, P2Y12 antagonists, statins, ACEIs/ARBs, and b-blockers, respectively, at discharge (Fig.S9). Among patients with at least one prescription filled, ATM of the PCI population and drug types of each medication class were determined, as shown in Fig.S10 and S11, respectively. Tables 2 and S1–S9 present the baseline characteristics of PCI population, CABG population, and conservative treatment population. In conservative treatment population, adherence to P2Y12 antagonists was significantly associated with age of patients (P<0.05).
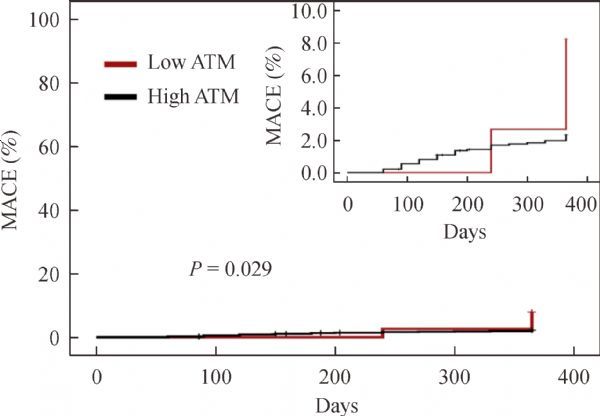
Fig.3 Estimated rates of MACE per adherence to P2Y12 antagonists in PCI population. The panel shows the outcomes for the PCI population. X-axis represents days after discharge, and Y-axis shows cumulative rates of MACE. The inset graph in each panel shows the same curves on a larger scale. MACE: major adverse cardiac events.
Table 3 and Figs. 3 and S12–S15 show that in patients undergoing PCI, only low adherence to P2Y12 antagonists was significantly associated with higher risk of MACE (P = 0.029). The difference remained significant after adjustment for potential confounders (HR, 0.172, 95% confidence interval: 0.039 to 0.763; P = 0.021).
This study shows high incidence rate of using medications for secondary prevention. Therefore, guideline-based therapies are strongly recommended for management of ACS to lower morbidity and mortality. Nevertheless, we observed that one year after discharge, more than one third of patients were no longer adherent to at least one medication. Adherence varies according to different medication classes, and our study revealed many characteristics associated with ATM. More importantly, we discovered that patients undergoing PCI with high adherence to P2Y12 antagonists were more susceptible to developing better outcomes.
To measure medication adherence, some tools, such as self-reported Morisky Score, were applied. However, considering that self-reported Morisky Score is limited in settings with low rate of nonadherence [11], we opted to use PDC to measure medication adherence.
In the present study, we noted that patients who underwent PCI were generally more prone to refilling their prescriptions for P2Y12 antagonists during the first year after discharge than patients with CABG. This result is similar to those described by Hlatky et al. [12]. Similarly, patients treated using conservative methods were more vulnerable to discontinue taking aspirin, P2Y12 antagonists, statins, or b-blockers; possibly, in non-PCI-treatments, preventive medications are less probable to be prescribed, and patients are encouraged to undergo subsequent follow-ups, whereas after PCI, patients are educated regarding the importance of medications, particularly DAPT, in maintaining stent thrombosis [12]. Furthermore, patients without revascularization might not regard their conditions as serious and hence think that some medications are no longer necessary. Khanderia et al. discovered that patients undergoing CABG had concerns about overuse and harms caused by prescribed drugs, and whether low ATM was correlated with social, economic, and demographic factors [13]. On the other hand, patients undergoing CABG accounted for a very small proportion of our study group, indicating that results should be used with caution. Further research is needed to understand the causes of low adherence in non-PCI-treated patients and to develop appropriate interventions to improve ATM.
Previous studies demonstrated that co-payments also impact adherence [14,15], whereas in the present study, ATM is not associated with medical insurance, which might be attributed to the complex procedure of reimbursement and relatively high co-payment. Absence of statistically significant association was possibly caused by insufficient power, with demographic information on medical insurance available in only half of the population. Nonetheless, all these studies suggest that more effort should be given to improve medical insurance in China.
Regimen complexity also contributes to ATM. Prior studies [16,17] mainly emphasized the dosing frequency and multi-drug regimens, whereas ours considered different drug types under each medication class (for example, ticagrelor and clopidogrel of P2Y12 antagonists) and revealed that the mainly used drugs under each medication class were not associated with ATM. This result possibly indicates that using preventive medications is not limited by different drug types when considering ATM only. Furthermore, we explored the associations between ATM and multi-drug regimens and observed that adherence to statins, ACEIs/ARBs, and b-blockers improved with aspirin application. Similar results were observed with P2Y12 antagonists, indicating the improvement in adherence to statins. Interestingly, in adjusted analysis, multiple drug therapy did not affect ATM. Patients with concomitant use of aspirin and P2Y12 antagonists were more prone to undergo PCI, which was strongly associated with ATM. Results remained nonsignificant in PCI-treated and non-PCI-treated patients. Another study by Gislason et al. also revealed a similar result in which the multi-drug regimens during the study period did not worsen long-term adherence. However, by contrast, adherence to b-blockers and statins improved. The researchers also found that early initiation of multiple drug treatment during the study period was not associated with decreased long-term compliance. Their results suggest that noncompliance was not associated with increased efforts to administer more medicines in more patients during the study period [4]. Nonetheless, our study suggests that ATM associated with multi-drug regimens may not be as destructive as implied in previous reports [18,19].
As shown in many studies, low ATM, particularly that for DES thrombosis, which result from low adherence to aspirin and P2Y12 antagonists, is deleterious [20,21]. However, Kimura et al. doubted the actual role of P2Y12 antagonists and aspirin in preventing stent thrombosis; since then, more reservations were allotted for the effect of low adherence to dual antiplatelet medication. Likewise, in another study [7], low adherence to antiplatelet drugs was not associated with MACE (ACS and cardiac death), and result was explained by temporal interruption of antiplatelet medication and negligible rate of antiplatelet medication discontinuation during the first month after stenting; the first month is considered the most deleterious period [18]. Notably, association of absence of risk of MACE with low ATM was also observed in ACS patients in the present study. However, given the differences in definitions of MACE and ATM, these results should be interpreted with caution. In the present study, low ATM was defined as PDC<50%, and discontinuation of medications was defined as a break for at least three months. Nevertheless, in PCI-treated patients, the absence of risk for low ATM was generally consistent, with an exception for higher adherence to P2Y12 antagonists associated with lower risk of MACE, as approximated by the study of Airoldi et al. [19]; in that particular study, discontinuation of P2Y12 antagonists was used to determine occurrence of stent thrombosis within the first six months.
Several limitations must be acknowledged upon evaluation of results from this observational study. First, PDC of some patients was not accurately assessed because of the vague interval from index date to the exact day of medication discontinuation, that is, the available data were only the time at which medication was discontinued at each time point of follow-up (1, 6, and 12 months after discharge). We arbitrarily classified the patients into low adherence (PDC<50%) and high adherence (PDC>50%) groups; most studies defined high adherence as PDC>80%. Second, the relatively low rate of events after discharge in low ATM patients weakened the power to make a strong statement regarding the risk of MACE. Furthermore, a potential recall bias possibly existed in follow-up information, i.e., repeated calls probably caused patients to be more adherent to medications, and hence the estimated rate of ATM could be lower than that in other contexts. Third, the present study lacked objective measures for medication use. Testing the urine or blood to confirm successful medication would yield better results. Furthermore, the present study is a single-center study, which might have also caused certain bias. Finally, confounding bias was also possible.
Our study suggests that non-PCI-treated patients are less likely to remain adherent to medications compared with patients who underwent PCI, and low adherence to P2Y12 antagonists in PCI-treated patients was associated with higher risk of MACE during the first year after discharge.
We want to acknowledge all the participants in this study, especially Profs. Jiangtao Yan, Jiangang Jiang, Hesong Zeng, and Xiamei Guo for their help in patient recruitment and also Drs. Xiang Nie, Yong Yang, Mengying He, Yuying Li, Qiang Huang, and Zhihui Chen for their contribution on the collection of medical records. This study was supported by grants from the National “973” program (No. 2012CB518004) and the Key Project of National Natural Science Foundation of China (No. 91439203). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have declared that no competing interests exist.
| 1 |
Gaziano TA, Opie LH, Weinstein MC. Cardiovascular disease prevention with a multidrug regimen in the developing world: a cost-effectiveness analysis. Lancet 2006; 368(9536): 679–686
DOI:10.1016/S0140-6736(06)69252-0
PMID:16920473
|
| 2 | Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP, Gencer B, Hasenfuss G, Kjeldsen K, Lancellotti P, Landmesser U, Mehilli J, Mukherjee D, Storey RF, Windecker S, Baumgartner H, Gaemperli O, Achenbach S, Agewall S, Badimon L, Baigent C, Bueno H, Bugiardini R, Carerj S, Casselman F, Cuisset T, Erol Ç, Fitzsimons D, Halle M, Hamm C, Hildick-Smith D, Huber K, Iliodromitis E, James S, Lewis BS, Lip GY, Piepoli MF, Richter D, Rosemann T, Sechtem U, Steg PG, Vrints C, Luis Zamorano J; Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016; 37(3): 267–315 PMID:26320110 |
| 3 |
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, Granger CB, Lange RA, Mack MJ, Mauri L, Mehran R, Mukherjee D, Newby LK, O’Gara PT, Sabatine MS, Smith PK, Smith SC Jr. 2016 ACC/AHA Guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2016; 68(10): 1082–1115
DOI:10.1016/j.jacc.2016.03.513
PMID:27036918
|
| 4 |
Gislason GH, Rasmussen JN, Abildstrøm SZ, Gadsbøll N, Buch P, Friberg J, Rasmussen S, Køber L, Stender S, Madsen M, Torp-Pedersen C. Long-term compliance with beta-blockers, angiotensin-converting enzyme inhibitors, and statins after acute myocardial infarction. Eur Heart J 2006; 27(10): 1153–1158
DOI:10.1093/eurheartj/ehi705
PMID:16399775
|
| 5 | Mathews R, Wang TY, Honeycutt E, Henry TD, Zettler M, Chang M, Fonarow GC, Peterson ED; TRANSLATE-ACS Study Investigators.Persistence with secondary prevention medications after acute myocardial infarction: Insights from the TRANSLATE-ACS study. Am Heart J 2015; 170(1): 62–69 PMID:26093865 |
| 6 |
Haukka J, Niskanen L, Partonen T, Lönnqvist J, Tiihonen J. Statin usage and all-cause and disease-specific mortality in a nationwide study. Pharmacoepidemiol Drug Saf 2012; 21(1): 61–69
DOI:10.1002/pds.2255
PMID:21956915
|
| 7 |
Ferreira-González I, Marsal JR, Ribera A, Permanyer-Miralda G, García-Del Blanco B, Martí G, Cascant P, Masotti-Centol M, Carrillo X, Mauri J, Batalla N, Larrousse E, Martín E, Serra A, Rumoroso JR, Ruiz-Salmerón R, de la Torre JM, Cequier A, Gómez-Hospital JA, Alfonso F, Martín-Yuste V, Sabatè M, García-Dorado D. Double antiplatelet therapy after drug-eluting stent implantation: risk associated with discontinuation within the first year. J Am Coll Cardiol 2012; 60(15): 1333–1339
DOI:10.1016/j.jacc.2012.04.057
PMID:22999716
|
| 8 |
Eagle KA, Kline-Rogers E, Goodman SG, Gurfinkel EP, Avezum A, Flather MD, Granger CB, Erickson S, White K, Steg PG. Adherence to evidence-based therapies after discharge for acute coronary syndromes: an ongoing prospective, observational study. Am J Med 2004; 117(2): 73–81
DOI:10.1016/j.amjmed.2003.12.041
PMID:15234641
|
| 9 | Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P, McFadden E, Lansky A, Hamon M, Krucoff MW, Serruys PW; Academic Research Consortium.Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 2007; 115(17): 2344–2351 PMID:17470709 |
| 10 |
Thygesen K, Alpert JS, White HD, Jaffe AS, Apple FS, Galvani M, Katus HA, Newby LK, Ravkilde J, Chaitman B, Clemmensen PM, Dellborg M, Hod H, Porela P, Underwood R, Bax JJ, Beller GA, Bonow R, Van der Wall EE, Bassand JP, Wijns W, Ferguson TB, Steg PG, Uretsky BF, Williams DO, Armstrong PW, Antman EM, Fox KA, Hamm CW, Ohman EM, Simoons ML, Poole-Wilson PA, Gurfinkel EP, Lopez-Sendon JL, Pais P, Mendis S, Zhu JR, Wallentin LC, Fernández-Avilés F, Fox KM, Parkhomenko AN, Priori SG, Tendera M, Voipio-Pulkki LM, Vahanian A, Camm AJ, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Morais J, Brener S, Harrington R, Morrow D, Lim M, Martinez-Rios MA, Steinhubl S, Levine GN, Gibler WB, Goff D, Tubaro M, Dudek D, Al-Attar N. Universal definition of myocardial infarction. Circulation 2007; 116(22): 2634–2653 doi:10.1161/CIRCULATIONAHA.107.187397
PMID:17951284
|
| 11 |
Shalansky SJ, Levy AR, Ignaszewski AP. Self-reported Morisky score for identifying nonadherence with cardiovascular medications. Ann Pharmacother 2004; 38(9): 1363–1368
DOI:10.1345/aph.1E071
PMID:15238622
|
| 12 |
Hlatky MA, Solomon MD, Shilane D, Leong TK, Brindis R, Go AS. Use of medications for secondary prevention after coronary bypass surgery compared with percutaneous coronary intervention. J Am Coll Cardiol 2013; 61(3): 295–301
DOI:10.1016/j.jacc.2012.10.018
PMID:23246391
|
| 13 |
Khanderia U, Townsend KA, Erickson SR, Vlasnik J, Prager RL, Eagle KA. Medication adherence following coronary artery bypass graft surgery: assessment of beliefs and attitudes. Ann Pharmacother 2008; 42(2): 192–199
DOI:10.1345/aph.1K497
PMID:18198242
|
| 14 | Doshi JA, Zhu J, Lee BY, Kimmel SE, Volpp KG. Impact of a prescription copayment increase on lipid-lowering medication adherence in veterans. Circulation 2009; 119(3): 390–397 |
| 15 |
Taira DA, Wong KS, Frech-Tamas F, Chung RS. Copayment level and compliance with antihypertensive medication: analysis and policy implications for managed care. Am J Manag Care 2006; 12(11): 678–683
PMID:17090224
|
| 16 |
Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther 2001; 23(8): 1296–1310
DOI:10.1016/S0149-2918(01)80109-0
PMID:11558866
|
| 17 |
Melloni C, Alexander KP, Ou FS, LaPointe NM, Roe MT, Newby LK, Baloch K, Ho PM, Rumsfeld JS, Peterson ED. Predictors of early discontinuation of evidence-based medicine after acute coronary syndrome. Am J Cardiol 2009; 104(2): 175–181
DOI:10.1016/j.amjcard.2009.03.013
PMID:19576342
|
| 18 | Spertus JA, Kettelkamp R, Vance C, Decker C, Jones PG, Rumsfeld JS, Messenger JC, Khanal S, Peterson ED, Bach RG, Krumholz HM, Cohen DJ. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: results from the PREMIER registry. Circulation 2006; 113(24): 2803–2809 |
| 19 | Airoldi F, Colombo A, Morici N, Latib A, Cosgrave J, Buellesfeld L, Bonizzoni E, Carlino M, Gerckens U, Godino C, Melzi G, Michev I, Montorfano M, Sangiorgi GM, Qasim A, Chieffo A, Briguori C, Grube E. Incidence and predictors of drug-eluting stent thrombosis during and after discontinuation of thienopyridine treatment. Circulation 2007; 116(7): 745–754 |
| 20 |
Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 2007; 297(2): 177–186
DOI:10.1001/jama.297.2.177
PMID:17213401
|
| 21 |
Thim T, Johansen MB, Chisholm GE, Schmidt M, Kaltoft A, Sørensen HT, Thuesen L, Kristensen SD, Bøtker HE, Krusell LR, Lassen JF, Thayssen P, Jensen LO, Tilsted HH, Maeng M. Clopidogrel discontinuation within the first year after coronary drug-eluting stent implantation: an observational study. BMC Cardiovasc Disord 2014; 14(1): 100
DOI:10.1186/1471-2261-14-100
PMID:25125079
|